Acid Reflux & Bloating - Gat Tea
Main menu:
- Home Page
- Buy here
- Introduction of Gat Tea
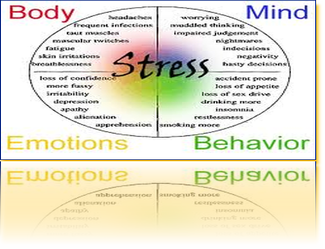
- Read About Stress
- Acid Reflux & Bloating
- Fibroids & Stress
- Diabetes Studies
- Gat Tea Herbs
- Gat Tea Youtube
- Gat Tea Blogs
- Contact information
-
Gat Tea Testimonies
- Gattea.tv Link
- Boo-Boo Honey
- Video testimonies
- Submitted testimonies
-
Cook Book Pictures
- Link to Cookbook pic
- Separator 5
- Page 22
Gat Tea
Much higher quality and better value than other tea brands
For IBS bloating and gas
* Loose tea or unbleached jumbo tea bags!
* Ingredients: organic fennel
* High volatile oil content ~ Whole seeds
Specs:
* Volatile Oil: 1.5% minimum
* Naturally caffeine-free
Interested in Gat Tea Tummy Tea? Get an even better deal with the
Gat Tea ~ A Medical Food for the Dietary Management of IBS
Clinical studies have shown that Herbs, as part of the diet, helps regulate contractions of the small intestine and aids gas expulsion. Fennel also relaxes the gut, which can relieve spasms of the GI tract. As a result, herbs assists in the dietary management of IBS symptoms, and is exceptional for IBS bloating, gas and abdominal pain. herbs is also a traditional digestive aid for colic, heartburn, indigestion, and stomachaches.
Gat Tea is packed in very generous quantities because it is meant to be used daily as a medical food for IBS; brew a delicious cup of tea several times a day, every day, as part of your dietary management of IBS symptoms.
Gat Tea is unique because it is formulated to contain a high volatile oil content and whole seed size (both factors are integral to the quality and potency of fennel and other herbs); it is harvested and packaged to be as fresh as possible; and it is processed for minimal volatile oil dissipation. It is the volatile oils in fennel that make it so effective for the dietary management of IBS symptoms, particularly bloating and gas.
Our fennel is certified and is guaranteed to be the freshest, strongest, and most delicious fennel tea available! If you're used to drinking fennel tea from store-bought tea bags, you'll find the difference in strength and taste of Gat Tea nothing short of astonishing.
Fennel's primary volatile oils are are anethole, fenchone, and estragole. Anethole is known to have a relaxing effect on the intestine. Fennel also has antioxidant and antimicrobial properties.
Fennel's documented use goes back to ancient China, and the plant is mentioned in virtually every European work on herbal medicines from ancient times to modern day. The mild licorice-flavored seeds are native to the Mediterranean, were known to the ancient Greeks, and were spread throughout Europe by Imperial Rome. In the 1st century A.D. Pliny attributed 22 healing properties to fennel. According to Chaucer, the 14th century English poet, fennel was one of the nine holy herbs of the Anglo-Saxons.
The United States once listed fennel as an official drug to be used for digestive problems, and today the herb is still used daily as an after-dinner digestive aid from India to Italy to Spain. Fennel is classified as GRAS (generally recognized as safe) by the FDA - there are no limitations on its use as a daily digestive aid. Fennel is so safe it's even used to treat infants with colic.
Brew Gat Tea Organic Fennel as teabags or as loose tea; for the loose tea, use any type of tea strainer, tea ball, or tea press. Brew with boiling water, but do not actually boil the teabags or loose tea in water as this can destroy its volatile oils, and thus its effectiveness. Fennel tea (like all of Gat Tea's) is naturally caffeine-free, as it does not contain any actual tea leaves (tea is a specific plant, even though other herbal drinks are commonly called "teas"). The stronger you brew this tea the more effective it will be. Lightly crushing the seeds before brewing them with hot water will increase their strength. The teabags are unbleached and organic-suitable.
Fennel tea can be sweetened with a little honey or plain sugar if you wish but I also think it's delicious plain. It can be chilled into iced tea, but remember that ice-cold beverages on an empty stomach can trigger GI spasms, whereas the heat in hot teas is in and of itself a muscle relaxant. The stronger the fennel tea, the more pronounced its beneficial effects on your digestion, so don't be afraid to make a dark brew!
* This product is a medical food for the dietary management of Irritable Bowel Syndrome (IBS), and is intended to be used under medical supervision.
Irritable Bowel Syndrome (IBS) SupplementsSupplements for the dietary management of IBS can be unbelievably helpful for stabilizing digestion. This is particularly true when they're used as one of the five key strategies for controlling Irritable Bowel Syndrome (proper diet, stress management, alternative therapies, and prescription medications are the other four).
Soluble fiber supplements, herbs that have medicinal effects on the gastrointestinal tract, heat therapy, probiotics, calcium and/or magnesium, and digestive enzymes are all of proven benefit. Best of all, results are usually felt very quickly - sometimes even immediately.
Most reputable Irritable Bowel Syndrome supplements are very safe and healthy overall (and they're usually inexpensive as well), so you definitely don't have much to lose by trying them.
Probiotics, such as acidophilus, are live cultures, and are available as pills or in soy yogurt (avoid dairy yogurt - see dietary trigger foods to learn why). Probiotics occur naturally in fermented foods.
The cultures help normalize and maintain healthy gastrointestinal flora, which can minimize diarrhea, bloating, gas, and painful abdominal cramps. Probiotics are most effective when they're taken in conjunction with a prebiotic; a prebiotic (such as Tummy Fiber Acacia) is something that encourages the growth of probiotics. Soluble fibers often have a prebiotic effect, as their normal fermentation in the gut causes the production of beneficial short-chain fatty acids, which then lead to the growth of good gut flora. This in turn leads to a reduction (sometimes dramatic) in abdominal bloating and gas.
Probiotics are particularly effective when your gut is under assault from antibiotics, though they can also be helpful when taken for daily maintenance. Quite a few research studies have shown that probiotics can dramatically improve irritable bowel syndrome. The problem is that other studies have found that many retail brands of probiotics don't actually contain any live cultures at all, and are thus worthless. Though probiotic supplements are widely available at drug and health food stores, it can be difficult to know if the brand you're buying is high quality and really does contain live cultures. Probiotic supplements should be taken with food.
Calcium and Magnesium play critical and antagonistic roles in regulating muscle function. Together they provide the mechanism for muscle contraction and relaxation.
In terms of GI tract function, calcium has a constipating effect, whereas magnesium acts as a laxative. As a result, calcium supplements can be truly beneficial for people with diarrhea-predominant IBS, and magnesium supplements can work wonders for IBS-constipation. Remember that calcium can block iron absorption in the body and contribute to anemia, so women who take calcium supplements may want to take an iron supplement at a different time of day. Calcium and magnesium should both be taken with food.
To take a calcium/magnesium supplement that will keep your bowel function in balance, it's typically recommended to use a 2:1 ratio of calcium to magnesium, as many people absorb magnesium more easily than calcium. I wouldn't exceed the USRDA for calcium or magnesium, taken either singly or together, without an explicit recommendation from your physician.
Digestive Enzymes can be helpful when taken right before a meal, especially if there is more fat in that meal than is safe for IBS. Enzymes are available at all health food stores and may be of more benefit to older people, as natural digestive enzyme production declines with age.
For gassy foods such as beans, lentils, and many vegetables, there is Beano, a brand-name digestive enzyme. Beano contains the sugar-digesting enzyme that the body needs (and which some people lack) to digest the complex sugar raffinose. If you have trouble digesting raffinose the sugar will ferment in your colon, producing gas and intestinal distress. Beano breaks down raffinose into simple sugars that cause no GI discomfort. Beano is available at health food stores in either tablets or drops, and is simply taken at the beginning of a meal. There are no side effects and the product can be used every day. To View Live Video Testimonys Click here www.gattea.tv
Gastroesophageal reflux disease
Peptic esophagitis; Reflux esophagitis; GERD; Heartburn - chronic; Dyspepsia - GERD
Gastroesophageal reflux disease (GERD) is a condition in which the stomach contents (food or liquid) leak backwards from the stomach into the esophagus (the tube from the mouth to the stomach). This action can irritate the esophagus, causing heartburn and other symptoms.
Causes, incidence, and risk factors
When you eat, food passes from the throat to the stomach through the esophagus (also called the food pipe or swallowing tube). Once food is in the stomach, a ring of muscle fibers prevents food from moving backward into the esophagus. These muscle fibers are called the lower esophageal sphincter, or LES.
If this sphincter muscle doesn't close well, food, liquid, and stomach acid can leak back into the esophagus. This is called reflux or gastroesophageal reflux. Reflux may cause symptoms, or it can even damage the esophagus.
The risk factors for reflux include:
•
Alcohol (possibly)
•
Hiatal hernia (a condition in which part of the stomach moves above the diaphragm, which is the muscle that separates the chest and abdominal cavities)
•
Obesity
•
Pregnancy
•
Scleroderma
•
Smoking
Heartburn and gastroesophageal reflux can be brought on or made worse by pregnancy and many different medications. Such drugs include:
•
Anticholinergics (e.g., for seasickness)
•
Beta-blockers for high blood pressure or heart disease
•
Bronchodilators for asthma
•
Calcium channel blockers for high blood pressure
•
Dopamine-active drugs for Parkinson's disease
•
Progestin for abnormal menstrual bleeding or birth control
•
Sedatives for insomnia or anxiety
•
Tricyclic antidepressants
If you suspect that one of your medications may be causing heartburn, talk to your doctor. Never change or stop a medication you take regularly without talking to your doctor.
Symptoms
More common symptoms are:
•
Feeling that food is stuck behind the breastbone
•
Heartburn or a burning pain in the chest (under the breastbone)
◦
Increased by bending, stooping, lying down, or eating
◦
More likely or worse at night
◦
Relieved by antacids
•
Nausea after eating
Less common symptoms are:
•
Bringing food back up (regurgitation)
•
Cough or wheezing
•
Difficulty swallowing
•
Hiccups
•
Hoarseness or change in voice
•
Sore throat